Trigeminal Neuralgia
Trigeminal neuralgia is a disorder of the trigeminal nerve that causes sudden, intense pain in your face. The trigeminal nerve (also called the 5th cranial nerve) is one of the largest nerves in your head. You have two trigeminal nerves, one on either side of your face. It is the trigeminal nerve that provides sensation in your face, detecting touch, pain, temperature and pressure sensations in the area between your jaw and forehead, including your lips and gums.
Trigeminal neuralgia usually affects only one side of your face, but rarely can it affect both sides, although not at the same time. If you have trigeminal neuralgia you will usually have episodes of sudden, intense, 'stabbing' pains in your face. Everyday activities like talking, eating, brushing your teeth or touching your face can trigger the pains. They usually last for several seconds and may be repeated one after the other. They may come and go throughout the day and last for days, weeks, or months, and then disappear for months or years. Over time, the period between attacks when you have no pain tends to become shorter.
Trigeminal neuralgia is also known as tic douloureux because the pain from the condition can be so intense that it causes a muscle spasm (twitch or jerk) in your face.
Trigeminal neuralgia affects about 5 in every 100,000 people. It is more common in women than men and usually affects people between 50 and 70 years old. Although infants, children and young adults can develop the condition, it is rare in people younger than 40.
Symptoms
The only symptom of trigeminal neuralgia is pain in your face that can last from a few seconds to about a minute. Between attacks of pain you have no other symptoms. Some people have mild, occasional pains, while others have frequent, severe pains. For some people the condition can progress so that their initial short, mild attacks become more severe and longer over time.
The pain is usually described as 'sharp', 'shooting', 'stabbing', 'jabbing', or 'like an electric shock'. It can be so severe that it can make the muscles in your face spasm (twitch or jerk), which is why the condition was previously known as 'tic douloureux', or 'painful tic'.
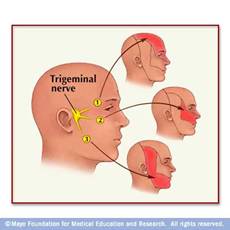
The trigeminal nerve is divided into three branches that travel through your face:
The first branch controls sensation in your eye, upper eyelid and forehead.
The second branch controls sensation in your lower eyelid, cheek, nostril, upper lip and upper gum.
The third branch controls sensation in your jaw, lower lip, lower gum and some of the muscles you use for chewing.
It is most common for the second and third branches of the trigeminal nerve to be affected. This means that the pain is usually around your cheek and jaw. It is less common for the first branch to be affected, so pain around your eye and on your forehead is less common. You may feel pain in the area controlled by just one branch of the trigeminal nerve, or the pain may affect all branches on one side of your face.
The pain may be triggered by:
touching your face,
talking or smiling,
eating or drinking,
brushing your teeth,
shaving, and
putting on makeup.
About half of those with trigeminal neuralgia have specific trigger points on their face, usually located between their lips and their nose, where pain can be triggered by a touch or even a change in temperature.
Trigeminal neuralgia is unpredictable. For unknown reasons, many people have periods where the condition suddenly gets worse and they have repeated painful episodes over several days, weeks or months. This can be followed by a pain-free period that lasts for months or even years. The frequency of pains varies from up to a hundred a day, to just an occasional pain every now and then. Sometimes you may feel a tingling or numbness before an attack.
Trigeminal neuralgia almost never occurs at night when you are sleeping.
Causes
Most cases of trigeminal neuralgia are thought to be caused by an abnormal blood vessel pressing on the trigeminal nerve, usually deep within your skull where the nerve attaches at the base of your brain. It is believed this irritates the nerve, triggering the pain. However, it is not known why blood vessels should start to press on the trigeminal nerve in later life.
Other less common reasons for the trigeminal nerve 'misfiring' include a tumour pressing on the nerve and a rare type of stroke. About 8% of people who have multiple sclerosis (MS) eventually develop trigeminal neuralgia due to the nerve damage that MS causes.
In some people with trigeminal neuralgia, the cause is unknown.
If you already have the condition it is known that stress can trigger an attack.
Diagnosis
Your doctor will diagnose trigeminal neuralgia based on your symptoms, a physical examination and medical tests.
They will ask you about your medical history and to describe your pain - how severe it is, what part of your face it affects, how long the pain lasts, and what triggers it. They will examine your head and neck, including the inside of your mouth, to try to find exactly where your pain is occurring and which parts of the trigeminal nerve may be affected.
Your doctor may ask you to have an MRI scan (magnetic resonance imaging scan) or CT scan (computerized tomography scan). These scans can show if a blood vessel or tumour is pressing on your trigeminal nerve. As there is no specific test for trigeminal neuralgia an important step in diagnosing the condition is ruling out other possible causes of your symptoms. These scans can help to rule out other possible causes.
Treatment
The most common treatment for trigeminal neuralgia is medication. This is often able to decrease or entirely block the pain signals that the trigeminal nerve sends to your brain. There are a number of medicines available, so if you stop responding to one drug, or if you experience too many side effects, your doctor may suggest that switch you to an alternative.
The anticonvulsant (medicine that prevents fits) drug carbamazepine is the drug most often used to treat trigeminal neuralgia. Carbamazepine eases pain within 24 hours for about 7 out of 10 people with the condition, and within 2 days for 9 out of 10.
Your doctor will start you on a low dose and gradually increase it until you reach a dose high enough to stop your pains. The dose needed varies from person to person. Most doctors recommend that you take carbamazepine until about a month after your pains have stopped. They may then gradually reduce your dose and eventually stop it altogether. Many people who take carbamazepine find they then have a period when they have no pains. However, the pains are likely to return at some point in the future, so treatment often needs to be restarted.
Some people find that carbamazepine works well at first but less well over time and about 1 in 10 people experience side effects. These can include dizziness, double vision, drowsiness and nausea. Side effects become more likely the higher the dose of carbamazepine you need to control the pains, but even low doses can cause side effects in some people. Quite often the side effects are only temporary, so it is worth persisting with the medication if your pains decrease and your side effects are not too bad.
About 20% of people with trigeminal neuralgia develop resistance to carbamazepine. Your doctor may prescribe other medicines if carbamazepine does not work well, if you develop a resistance, or if it causes severe side effects. Alternatives include other anticonvulsants such as gabapentin and amitriptyline. Sometimes your doctor may prescribe a combination of two medicines if one alone does not help.
Some people with trigeminal neuralgia eventually stop responding to medication, or they experience unacceptable side effects. For these people, surgery - or a combination of surgery and medication - may be an option.
There are a variety of surgical procedures used to treat trigeminal neuralgia:
Rhizolysis
In this approach, part of your trigeminal nerve is damaged or destroyed to block the electrical activity in the nerve that is causing your pain. Inserting a Radiofrequency needle and causing a thermocoagulation lesion or injecting the chemical glycerol or alcohol into the trigeminal nerve can achieve this. Or a tiny balloon can be injected through a hollow tube inserted through the skin of your cheek and then inflated to damage the nerve. These procedures give immediate pain relief to almost all people, but between 25-50% of people will find the condition returns. You may need the procedure repeated, or to have a different procedure. And because this surgery is designed to damage the nerve, a possible side effect is permanent numbness to part of your face.
Microvascular decompression - this approach may be used if your doctor finds that your trigeminal neuralgia is caused by a blood vessel pressing on the trigeminal nerve. A surgeon will open your skull behind your ear so that they can see the nerve. They will then find the blood vessel that is pressing on the nerve and lift it away. The success rate for this procedure is about 90% and 70-80% of people experience permanent pain relief. A possible side effect of this procedure is permanent numbness in a part of your face.
Stereotactic radiosurgery
In this approach, beams of radiation are used to target the trigeminal nerve where it leaves your brain, without the need for any incision (cut). The procedure is fairly new and its long-term success rate is still being assessed, but it is expected to be successful for 85-90% of patients who undergo it. Only a few UK hospitals offer the procedure at the moment, but it has the advantage that it leads to permanent facial numbness in less than 10% of patients and less than 10% of patients find that their pain returns.
Complications
Anaesthetica dolorosa is the most morbid of complications. This is when there is complete numbness of the face but the patient still has pain. This is very difficult to treat but thankfully is rare. It is more likely to occur with the percutaneous procedures such as Radiofrequency ablation or glycerol injection.
If you have trigeminal neuralgia the pain can be so severe that it prevents you from eating and sleeping normally. This can lead to sleep deprivation, under-eating and even malnutrition, and occasionally people may need to be hospitalized due to weight loss and dehydration.
The level of pain, never knowing when the next pain is going to come, lack of sleep or under-eating, can also make people with trigeminal neuralgia irritable, anxious or depressed.